梁世傑:當“肝風”遇上“瘀水”,古方如何破解高血壓難題
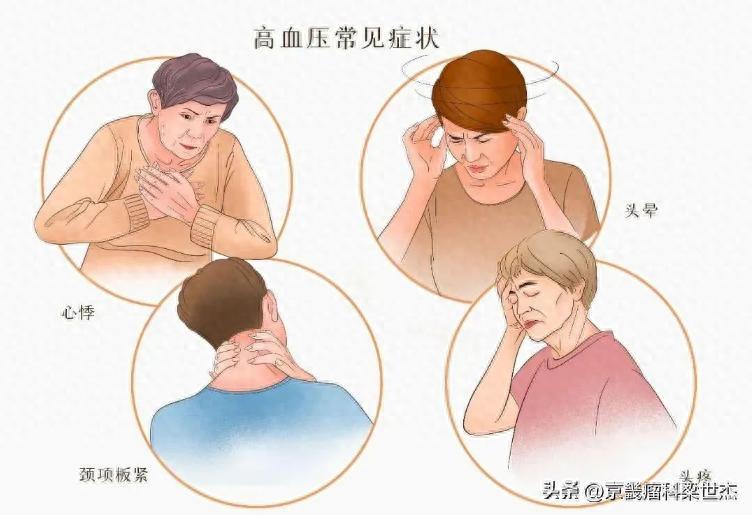
頭暈如坐舟車,頭痛似要裂開,身體莫名腫脹——高血壓帶來的困擾不僅僅是血壓計上冰冷的數字。
一位高血壓患者走進診室,他的困擾不僅是血壓計上顯示的160/100 mmHg,更是那些日夜折磨的症狀:頭暈時如坐舟船,頭痛似有錐刺,下肢水腫按之凹陷。
現代醫學給出了一線降壓藥方案,血壓雖有下降,但症狀改善有限。而一套包含天麻鉤藤飲、鎮肝熄風湯和桃核承氣湯的中醫組合方案,卻讓這位患者的症狀得到明顯緩解。
---
01 高血壓病理探微,千年醫學與現代科學的對話
高血壓早已成爲全球公共衛生挑戰。2019年數據顯示,全球30-79歲成年人中,男性高血壓患病率達34%,女性達32%。由於人口增長和老齡化,高血壓患者人數在三十年間翻了一番,從6.48億增加到12.78億。
現代醫學將高血壓定義爲血壓持續升高,最新指南甚至建議更早干預和更嚴格的控制目標,尤其對於心血管風險高的個體。當血壓驟升至180/110毫米汞柱或更高時,可能危及生命,需要緊急處理。
然而在中醫理論體系中,並沒有“高血壓”這一病名。中醫通過“辨證論治”,根據患者表現出的具體症狀羣來確定治療方向。
對於出現頭痛、眩暈等症狀的高血壓,中醫常將其歸爲“肝陽上亢”的範疇。簡單理解,就是身體上部“陽氣”過盛,如同自然界中樹木生長過旺,枝葉繁茂但根基不穩。
更復雜的情況是,這種“上盛”往往伴隨着“下虛”——肝腎陰液不足,無法制約陽氣。或如文章開頭提到的患者,在肝陽上亢的基礎上,還出現了“水腫”,中醫認爲這與“水溼停滯”、“瘀血內阻”密切相關。
02 經典方劑解析,三張古方的現代使命
面對複雜的高血壓病症,中醫發展出了多首經典方劑。針對“肝陽上亢”這一核心病機,天麻鉤藤飲和鎮肝熄風湯是兩張代表性處方。
天麻鉤藤飲,其藥物組成體現了“平肝潛陽,清熱安神”的治法。方中天麻、鉤藤爲君藥,專門平息上亢的肝陽;石決明增強平肝潛陽之力;梔子、黃芩清瀉肝經之熱。
這些藥材協同作用,專門用於治療肝陽上亢引起的頭痛、眩暈、耳鳴、眼花、失眠等症狀。研究表明,該方不僅能降低血壓,還能提升患者體內的抗氧化酶活性,具有多重保護作用。
鎮肝熄風湯則更側重於“鎮肝”與“滋陰”並重。它重用懷牛膝引血下行,代赭石、龍骨、牡蠣等礦物藥質量沉降,鎮逆肝陽;同時配伍龜板、白芍等滋養陰液,從根本補充肝腎不足。
臨牀觀察證實,鎮肝熄風湯治療肝陽上亢型高血壓有明確療效。當患者除頭暈頭痛外,還伴有面色潮紅、脾氣急躁等“陽亢”特徵明顯時,此方常被選用。
那麼,當高血壓患者出現“水腫”這一難題時,中醫又該如何應對?這便引入了第三張方劑——桃核承氣湯。
此方源自東漢張仲景的《傷寒論》,本用於治療“下焦蓄血”證。方中桃仁活血化瘀,大黃瀉下通便、活血祛瘀,桂枝通陽化氣,芒硝軟堅散結,甘草調和諸藥。
現代中醫發現,對於高血壓伴隨的瘀血與水溼互結狀態(表現爲水腫、舌質紫暗、口乾不欲飲等),桃核承氣湯能通過活血利水,改善微循環,消除水腫。
03 組合策略,古方聯用的協同智慧
單一古方往往難以應對複雜的高血壓病機。臨牀中,中醫師會根據患者具體情況,將不同方劑化裁組合。
例如,對於肝陽上亢明顯且伴有水腫的患者,可能會天麻鉤藤飲與桃核承氣湯合方。前者平抑肝陽、緩解頭暈頭痛;後者活血利水、消除下肢水腫。二者協同,標本兼治。
若患者陰虛徵象顯著,表現爲腰膝痠軟、口乾舌燥,則可能鎮肝熄風湯與桃核承氣湯合用。一者滋陰潛陽治其本,一者活血利水治其標。
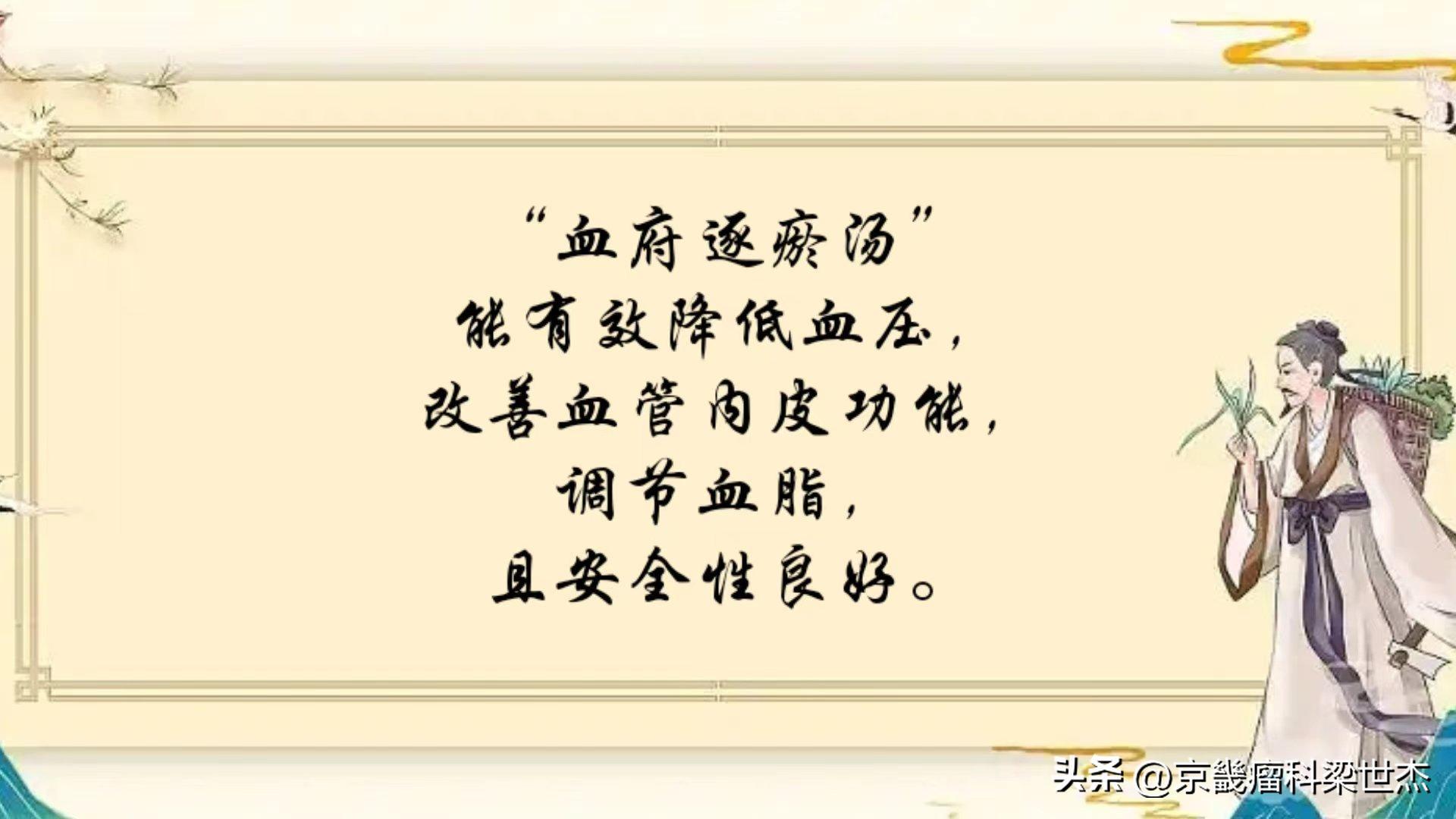
最新研究爲這類“活血化瘀”方劑治療高血壓提供了科學支持。一項納入37項研究、3391名患者的Meta分析表明,經典活血化瘀方“血府逐瘀湯”能有效降低血壓,改善血管內皮功能,調節血脂,且安全性良好。
這間接印證了在高血壓治療中,針對“瘀血”這一病機使用活血化瘀藥物的合理性與有效性。桃核承氣湯作爲活血化瘀的代表方之一,其作用機制與此有相通之處。
04 現代視角,中西醫協同的現實意義
面對高血壓這一健康殺手,2024年歐洲心臟病學會指南提出了新分類:非升高血壓(診室血壓<120/70 mmHg)、升高血壓(120-139/70-89 mmHg)和高血壓(≥140/90 mmHg)。
對於明確的高血壓,現代醫學主張多數人應儘快確診並開始藥物治療。一線藥物包括血管緊張素轉換酶抑制劑、血管緊張素Ⅱ受體阻滯劑、鈣通道阻滯劑和噻嗪類利尿劑等。
個別患者擔心使用口服降壓西藥終身服藥,這種情況下可以先服中藥治療,如療效比較好,能降至正常,則不用喫西藥降壓藥,假如控制不好,不能使血壓明顯下降,則應當及是。配合西醫治療,並勤量血壓。
中醫古方與現代降壓藥並非對立關係,而可能形成互補。對於使用西藥後血壓達標但症狀(如頭暈、頭痛、水腫)改善不理想的患者,在專業醫師指導下,配合中醫辨證論治,使用合適的方劑組合,可提高整體療效和生活質量。
中藥與西藥聯合應用時,更需注意潛在的相互作用,應在醫生和藥師指導下進行,切不可自行配藥服用。
附
梁世傑醫生高血壓驗方(肝陽上亢實證)收縮壓、舒張壓升高通治方:26味藥(天麻鉤藤飲合鎮肝熄風湯加桃核承氣湯)功效:平肝潛陽,活血化瘀,利水消腫。症見頭暈,頭疼,情緒煩躁易怒,腿腫腳腫,口乾舌燥,腰膝痠軟,疼痛,無力等症見真陰不足,上盛下虛、真火離位,肝陽上亢者。(處方藥量在醫師指導下使用,避免盲目套用)
天麻10克,鉤藤25克,石決明30克,生磁石30克,川牛膝15克,夏枯草30克,茺蔚子30克,車前子30克,紅花10克,槐花10克,黃芩15克,桃仁30克,生大黃10克,生地20克,芒硝6克,肉桂5克,生龍骨30克,生牡蠣30克,茵陳30克,天冬20克,麥冬20克,元參30克,川楝子15克,生梔子15克,炒杜仲20克,生赭石30克。
作者簡介:梁世傑 原首都醫科大學中醫門診部中醫主治醫師,京畿瘤科創始人,本科學歷,從事中醫臨牀工作25年,積累了較豐富的臨牀經驗。師從首都醫科大學附屬北京中醫院肝病科主任醫師、著名老中醫陳勇,侍診多載,深得器重,盡得真傳!擅用“商湯經方分類療法”、專病專方結合“焦樹德學術思想”“關幼波十綱辨證”學術思想治療疑難雜症爲特色。現任北京樹德堂中醫研究院研究員,北京中醫藥薪火傳承新3+3工程—焦樹德門人(陳勇)傳承工作站研究員,國際易聯易學與養生專委會常務理事,中國中醫藥研究促進會焦樹德學術傳承專業委員會委員,中國藥文化研究會中醫藥慢病防治分會首批癌症領域入庫專家。榮獲2020年中國中醫藥研究促進會仲景醫學分會舉辦的第八屆醫聖仲景南陽論壇“經方名醫”榮譽稱號。2023年首屆京津冀“扁鵲杯”燕趙醫學研究主題徵文優秀獎獲得者。事蹟入選《當代科學家》雜誌、《中華英才》雜誌。
Hypertension: When "Liver Wind" Meets "Blood Stasis," How Does Ancient Prescription Solve Thousand-Year-old Problem?
Dizziness as if riding in a boat, headache as if to split open, body swelling inexplicably - the troubles brought by high blood pressure are not just the cold numbers on the blood pressure gauge.
A hypertensive patient walked into the clinic, his troubles were not only the 160/100 mmHg displayed on the sphygmomanometer, but also those symptoms that tormented him day and night: dizziness like being on a boat, headaches like having a needle prick, lower limb edema that sank when pressed.
Modern medicine has given a line of antihypertensive drugs, although blood pressure has decreased, but the improvement of symptoms is limited. However, a combination of traditional Chinese medicine including Tianma Gouteng Decoction, Zhengan Xifeng Decoction and Taohuzhengqi Decoction significantly alleviated the patient''s symptoms.
---
Exploration of Pathology of Hypertension, Dialogue between Medicine of Thousands of Years and Modern Science
Hypertension has long been a global public health challenge. Data from 2019 shows that among adults aged 30-79 worldwide, 34% of men and 32% of women have high blood pressure. Due to population growth and aging, the number of people with hypertension has doubled in three decades, from 648 million to 1.278 billion.
Hypertension is defined as persistently elevated blood pressure, and recent guidelines even recommend earlier intervention and more stringent control targets, especially for individuals with high cardiovascular risk. When blood pressure rises abruptly to 180 / 110 mmHg or higher, it can be life-threatening and requires urgent treatment.
However, in the TCM theory system, there is no such disease as "hypertension." TCM determines the treatment direction based on the specific symptom group exhibited by patients through "differential diagnosis and treatment."
For hypertension with symptoms such as headache and dizziness, traditional Chinese medicine often classifies it into the category of "liver yang hyperactivity." Simply put, it means that there is too much "yang energy" in the upper part of the body, just like trees growing too much in nature, with lush branches and leaves but unstable roots.
In more complicated cases, this "excess of yang" is often accompanied by "deficiency of yin" - insufficient liver and kidney yin fluid to restrain yang qi. Or as mentioned at the beginning of the article, patients with hyperactivity of liver yang have also developed "edema," which traditional Chinese medicine believes is closely related to "stagnation of water and dampness" and "blood stasis."
02 Classic Prescription Analysis, The Modern Mission of Three Ancient Formulas
In response to complex hypertension, traditional Chinese medicine has developed many classic prescriptions. For "Liver Yang Rising," Tianma Gouteng Decoction and Zhen Gan Xi Feng Decoction are two representative prescriptions.
Tianma Gouteng Decoction, its drug composition reflects the "calming liver and subduing yang, clearing heat and calming spirit" treatment method. In the formula, Tianma and Gouteng are the main drugs, specifically to calm the excessive liver yang; Shijieding enhances the ability to calm the liver and subdue yang; Chrysanthemum and Scutellaria clear away the heat in the liver channel.
These medicinal herbs work synergistically to specifically treat symptoms such as headaches, dizziness, tinnitus, blurred vision, insomnia caused by hyperactivity of liver yang. Studies have shown that this formula not only lowers blood pressure but also enhances the activity of antioxidant enzymes in patients and has multiple protective effects.
Zhen Gan Jie Feng Tang is more focused on "calming the liver" and "nourishing yin." It uses Huai Niu Xi to guide blood downward, along with minerals such as Zhe Shi, Long Gu, and牡蠣 for sedimentation, to calm liver yang; at the same time, it combines turtle shell and White Peony Root to nourish yin fluid, fundamentally supplementing liver and kidney deficiency.
Clinical observation confirms that Zhen Gan Xi Feng Decoction has definite curative effect in treating hypertension with liver yang hyperactivity. When patients have symptoms such as dizziness and headache, accompanied by facial flushing and irritable temperament, this prescription is often chosen.
So, when hypertensive patients have the problem of "edema," how should traditional Chinese medicine deal with it? This brings us to the third formula - Taohuzhengqi Decoction.
This formula originated from Zhang Zhongjing''s "Treatise on Febrile Diseases" in the Eastern Han Dynasty, and was originally used for treating "accumulation of blood in the lower jiao." The formula includes persimmon seed to promote blood circulation and remove blood stasis, rhubarb to relieve constipation and remove blood stasis, cinnamon to promote yang and dispel gas, mirabilite to soften and disperse nodules, and licorice to harmonize all the herbs.
Modern TCM has found that for hypertension accompanied by blood stasis and water dampness (manifested as edema, purple tongue, dry mouth without desire to drink, etc.), Taohua Zhengqi Decoction can improve microcirculation through promoting blood circulation and diuresis to eliminate edema.
03 Combination Strategy, Synergetic Wisdom of Ancient Prescription Combination
It is often difficult for a single formula to cope with the complex pathogenesis of hypertension. In clinical practice, acupuncturists will combine different prescriptions according to the patient''s specific condition.
For example, for patients with obvious liver yang hyperactivity accompanied by edema, Tianma Gouteng Decoction and Taohuzhengqi Decoction may be combined. The former calms the liver yin and relieves dizziness and headaches; the latter promotes blood circulation and eliminates water retention in the lower limbs. Both work together to treat both the symptoms and root causes.
If the patient has significant symptoms of yin deficiency, characterized by weakness in the waist and knees, dry mouth and tongue, then it may be appropriate to use Zhen Gan Fu Feng Decoction combined with Taohuzhengqi Decoction. The first one nourishes yin and subdues yang to treat its root cause, while the second one promotes blood circulation and removes water to treat its surface symptoms.
The latest research provides scientific support for this type of "promoting blood circulation and removing blood stasis" formula to treat hypertension. A meta-analysis involving 37 studies and 3,391 patients showed that the classic promoting blood circulation and removing blood stasis formula "Xuefu Zhuyu Decoction" can effectively reduce blood pressure, improve vascular endothelial function, regulate blood lipids, and has good safety.
This indirectly confirms the rationality and effectiveness of using blood-activating and stasis-dispersing drugs in the treatment of hypertension based on the pathogenic mechanism of "blood stasis." Tao Zhu Cheng Qi Decoction, as one of the representative prescriptions for blood-activating and stasis-dispersing, has a similar mechanism of action to this.
04 Modern Perspectives and the Practical Significance of Sino-Western Medicine Collaboration
Faced with this health killer, the 2024 European Society of Cardiology guidelines propose a new classification: non-elevated blood pressure (office blood pressure < 120 / 70 mmHg), elevated blood pressure (120-139 / 70-89 mmHg) and hypertension (≥ 140 / 90 mmHg).
For clear hypertension, modern medicine advocates that most people should be diagnosed as soon as possible and start drug treatment. The first-line drugs include angiotensin converting enzyme inhibitors, angiotensin II receptor blockers, calcium channel blockers and thiazide diuretics.
Some patients worry about taking oral antihypertensive drugs for life, in which case they can first take Chinese medicine for treatment. If the effect is better and it can be reduced to normal, they do not need to take Western antihypertensive drugs. If control is not good and blood pressure cannot be significantly lowered, it should be done immediately. Cooperate with Western medicine treatment, and measure blood pressure frequently.
Traditional Chinese medicine and modern antihypertensive drugs do not have an opposing relationship, but may form a complementary relationship. For patients who have achieved blood pressure targets after using Western medicine but have unsatisfactory improvement in symptoms (such as dizziness, headache, and edema), under the guidance of professional physicians, combined with traditional Chinese medicine syndrome differentiation and treatment, appropriate combination of prescriptions can improve overall efficacy and quality of life.
When Chinese medicine and Western medicine are used together, it is necessary to pay more attention to potential interactions and should be done under the guidance of doctors and pharmacists, not self-medicating.
attach
Dr. Liang Shi-jie’s Prescription for Hypertension (Pathological Condition of Hyperactive Liver Yang): Increased systolic and diastolic pressures. Treatment formula: 26 herbs (Tianmao Jiuteng Decoction combined with Zhengan Xie Feng Decoction and Taohuo Chengqi Decoction). Effect: Balancing the liver and subduing yang, promoting blood circulation, detoxifying, and diuretic. Symptoms include dizziness, headaches, irritability, leg and foot swelling, dry mouth and tongue, weakness in the waist and knees, and pain. This prescription is suitable for individuals with insufficient true yin, excess energy above and deficiency below, and hyperactive liver yang. (The dosage of prescription drugs should be used under the guidance of a physician and not blindly replicated.)
10 grams of Tianma, 25 grams of Huo-teng, 30 grams of Shi-ju-ming, 30 grams of Sheng-qi-shi, 15 grams of Chuan-niu-xi, 30 grams of Xiao-kuo-cao, 30 grams of Cheng-wei-zi, 30 grams of Qian-che-zi, 10 grams of Hong-hua, 10 grams of Huai-hua, 15 grams of Huang-qin, 30 grams of Tao-ren, 10 grams of Sheng-da-huang, 20 grams of Sheng-di-ye, 6 grams of Mang-xiao, 5 grams of Rou-gui, 30 grams of Shen-long-guang, 30 grams of Sheng-mao-li, 30 grams of Yin-chen, 20 grams of Tian-dong, 20 grams of Mai-dong, 30 grams of Yuan-shen, 15 grams of Chu-lian-zi, 15 grams of Sheng-zhi-zi, 20 grams of Cha-du-zhong, and 30 grams of Sheng-ze-shi.
Author profile: Liang Shi-jie was a chief physician of traditional Chinese medicine at the Traditional Chinese Medicine Outpatient Clinic of Capital Medical University. He was the founder of Jingyi Tumor Clinic. He holds a bachelor’s degree and has been engaged in clinical work in traditional Chinese medicine for 25 years, accumulating extensive clinical experience. He studied under Chen Yong, a renowned senior traditional Chinese medicine practitioner at the Hepatology Department of Beijing Traditional Chinese Medicine Hospital affiliated to Capital Medical University. Over the years, he gained great respect and acquired genuine expertise. He specializes in using the “Shang Tang Classic Classification Therapy” and combining specific treatments for specific diseases with the “Jiao Shu-de Academic Thought” and the “Guan You-bo Ten-Principle Diagnosis” approach to treat complex medical conditions. He is currently a researcher at the Beijing Shu-de-Tang Traditional Chinese Medicine Research Institute and a researcher at the Beijing New 3+3 Project for the Inheritance of Traditional Chinese Medicine – Jiao Shu-de’s Disciples (Chen Yong) Heritage Workstation. He is a Standing director of the International Yi-lian Yi-xue and Health Preservation Committee and a member of the Committee for the Inheritance of Jiao Shu-de’s Academic Thought of the China Research Promotion Association for Traditional Chinese Medicine. He is also a member of the inaugural Cancer Expert Pool of the China Cultural Research Association for Traditional Chinese Medicine’s Prevention of Chronic Diseases. He was awarded the title of “Expert in Classic Prescriptions” at the Eighth Nanyang Forum of the Zhang Zhongjing Medical Division of the China Research Promotion Association in 2020. In 2023, he won the Excellence Award in the First Beijing-Tianjin-Hebei “Bian Que Cup” Yan-Zhao Medical Research Theme Essay Competition. His achievements have been featured in the magazines “Contemporary Scientists” and “China’s Elite”.